Recent shifts in pain management are reshaping conversations between doctors and patients. Traditionally, treatment options for chronic pain involved a step-by-step approach, often leading to frustration. Now, both patients and healthcare providers are increasingly considering alternative therapies, including cannabis, as part of a broader strategy to manage long-term pain.
Changing Perspectives on Pain Treatment
Living with chronic pain can severely affect daily activities such as dressing, walking, or even sitting still. For many individuals, the goal is not to find a miraculous cure but to discover effective ways to cope with pain on a daily basis. As a result, cannabis is no longer viewed as a singular solution; instead, it is regarded as one component among various medical approaches that can be integrated into existing treatment plans.
Typically, discussions about cannabis arise later in consultations, after patients have explored conventional methods such as medications, injections, physiotherapy, or even surgery. When these options fail to provide relief, cannabis may be introduced as a potential adjunct to ongoing therapies. This shift in dialogue empowers patients, offering them an additional avenue to explore rather than accepting a status quo of enduring pain.
Evaluating Private Pain Clinics
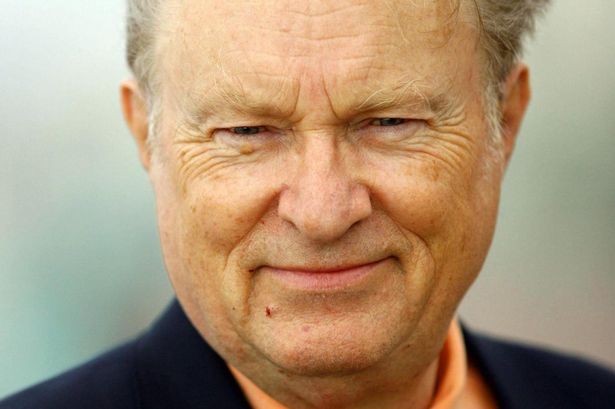
As patients begin to seek alternatives beyond the National Health Service (NHS), they often have straightforward inquiries. Critical questions focus on costs, clinic personnel, and the processes following initial appointments. For instance, many prospective patients wonder if treatment through private clinics, like Alternaleaf, presents a viable option.
What patients typically seek is clarity. They want to understand whom they will interact with, the extent of follow-up care, and whether there is adequate medical oversight. Transparent answers are essential for patients to determine if a clinic is a sensible choice or merely an appealing option that lacks substance.
The approach to pain management has evolved from a straightforward path of medication trials to a more nuanced exploration of various treatments. For some, traditional methods remain effective, while others continue to struggle with persistent pain that disrupts sleep and daily functioning. Consequently, the dynamic between doctors and patients is shifting towards a more collaborative exploration of different management strategies.
Understanding Cannabis Within Clinical Guidelines
In the UK, cannabis is integrated into pain management discussions under strict clinical guidelines. This means that its introduction into treatment plans is not arbitrary but based on established protocols, particularly for chronic pain cases where other treatments have proven ineffective. Prescribing cannabis is limited to specific conditions and is subject to careful consideration by medical professionals.
Importantly, cannabis is not positioned as a first-line treatment or a universal solution for all patients. Instead, it emerges as part of a more comprehensive conversation among healthcare providers when standard care fails to alleviate pain. This new framework alters the tone of consultations, shifting the focus from an absence of options to the potential for supplementary treatments under professional supervision.
Despite the growing interest in cannabis, pain specialists remain cautious. They emphasize that evidence regarding its efficacy is mixed. Individual responses vary significantly, and some patients may experience little to no benefit. This cautious optimism shapes the way cannabis is discussed in clinical settings, ensuring that it is not perceived as a panacea but rather as a possible adjunct for a select group of patients.
In practice, cannabis treatment is closely monitored, with adjustments made based on patient response. Progress is regularly assessed, and treatments can be halted if they do not yield the desired effects. This realistic approach helps maintain grounded discussions around pain management, avoiding unrealistic expectations.
While conversations about pain management are evolving, the decisions regarding treatment remain deeply personal. Chronic pain continues to be a persistent challenge for many individuals, influencing their quality of life. The willingness of healthcare providers to engage in discussions about alternative coping strategies represents a significant shift in approach. Although not every option is suitable for every patient, the dialogue is now more open and inclusive, allowing for a thoughtful exploration of what might help.
For those grappling with daily pain, this shift can provide a sense of relief. While it does not guarantee a cure, it fosters a more informed and nuanced conversation about potential treatment pathways, ultimately empowering patients to navigate their pain management journeys with greater confidence.