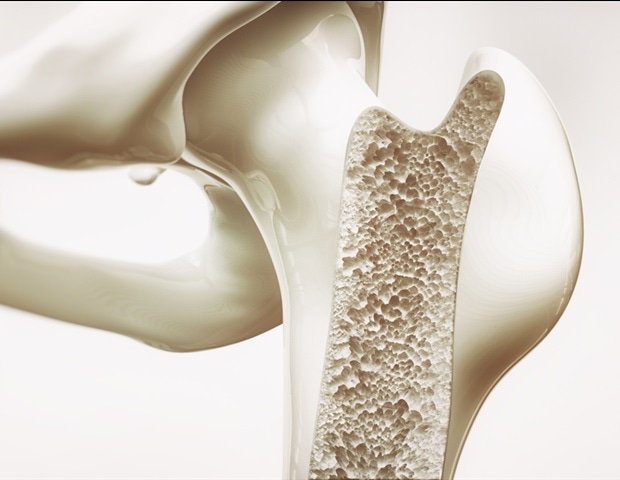
Advancements in MRI technology could significantly alter how medical professionals monitor the healing of broken bones. A new initiative, led by mechanical engineer Michael Hast from the University of Delaware, is set to develop innovative imaging techniques that promise to identify complications in bone healing earlier than traditional methods allow. The five-year project, backed by a grant of approximately $3 million from the National Institutes of Health (NIH), aims to enhance patient care by providing more timely insights into recovery progress.
Patients with broken bones typically undergo periodic X-rays to assess healing. This process can be time-consuming, often resulting in delays in clinical decision-making. Research indicates that healing of shin bone, or tibial, fractures may slow or stall in up to 25% of cases due to various factors, including age and underlying health conditions such as diabetes. These delays can lead to chronic pain and further medical complications.
Revolutionizing Imaging Techniques
Hast’s project focuses on developing radiation-free imaging techniques to assess bone healing more efficiently. Traditional methods, including computed tomography (CT) scans, expose patients to ionizing radiation, posing risks with frequent use. Recent advancements in magnetic resonance imaging (MRI) technology, particularly the ultrashort echo time MRI, allow researchers to capture detailed images of dense bone structures without harmful radiation exposure.
This innovative approach could be transformative. Hast stated, “With enough data, we should be able to identify problems with fracture healing much earlier. This could guide treatment decisions, such as adjusting physical therapy routines or activity levels.”
Collaborating with experts from Lehigh University and surgeons at the University of Pennsylvania, Hast’s team will use three-dimensional computational models to estimate the strength of healing bones. By mapping MRI data to the mechanical properties of bone, they aim to create a model that accurately reflects real-world conditions and stressors.
Future Implications for Patient Care
The research will initially utilize a sheep model of bone healing to verify the accuracy of MRI-based models against laboratory measurements. Subsequently, the team plans to enroll approximately 50 participants who have undergone tibial fracture repair surgery at the University of Pennsylvania. Each participant will be tracked over the course of a year to evaluate long-term recovery outcomes.
As recovery protocols evolve, Hast emphasizes the importance of early intervention. “A better predictive tool could give clinicians and patients more confidence that a healing bone can handle the stress of physical activity without risking a repeat fracture,” he remarked.
The project, funded by NIH’s National Institute of Arthritis and Musculoskeletal and Skin Diseases under award number AR083052, aims to refine rehabilitation approaches based on the insights gained from MRI data. The ultimate goal is to empower healthcare providers to respond proactively to potential healing issues, improving recovery times and overall patient outcomes.
With continued research and development, these new imaging techniques represent a significant step forward in the management of bone healing, potentially changing how clinicians approach fracture recovery in the years to come.